Welcome back!
This week, I’m writing from a new coffee shop in Brighton with the most acidic cold brew I’ve ever had. I’m here to talk about Shit Life Syndrome and my continuous disappointment in mental health.
Disclaimer, as usual: This newsletter is a notebook guided by my curiosity, not a scientific publication. Nothing is “scientifically” verified; everything could be true or false, or we could believe in different versions of truth. I welcome discussion!
Shit Life Syndrome came up when I was catching up with a friend. It wasn’t the first time income and being depressed were discussed in the same conversation. Still, the fact that it was coined in such a scientific way surprised me.
Here’s how Wikipedia describes it: “Shit life syndrome (SLS) is a phrase used by physicians in the United Kingdom, the United States, and Australia for the effect that a variety of poverty or abuse-induced disorders can have on patients.” Similarly, this article said that UK physicians sometimes wrote “SLS” as a diagnosis when they see a patient with so many socioeconomical disadvantages that medical interventions cannot help with.
Wikipedia then led me to the term “Disease of Despair,” which refers to the despair people feel when they feel that “their long-term social and economic prospects are bleak.” Common death outcomes of diseases of despair (termed “Deaths of Despair”) include suicide, drug overdose, and alcoholic liver diseases. Two of the three fall under mental/behavioral health outcomes. Basically, together, Shit Life Syndrome is a fancy term for patients suffering from poverty/socieconomic inequalities.
Reddit, which I sometimes use to gauge public opinion had a thread on Shit Life Syndrome that sparked debates over whether reactions to situations like bereavement and job loss necessitate SSRI medication. Another one talked about their frustrations as their therapist called their realization that they have a shit life “avoidant depression,” and questioned if therapists know how to treat Shit Life Syndrome at all. As always, I felt affirmed by Reddit, knowing I’m not the only one who thinks we should pay more attention to social determinants (which hopefully isn’t just a result of an algorithm).
To be clear, I don’t think I have Shit Life Syndrome— I believe my own mental health problems are more of “post-modernism angst” (i.e. being in a capitalistic society etc). I’m looking at it as a phenomenon, and my reactions to it surround the implications in psychiatry.
First, it is funny that such an intuitive concept had such a biological name (“syndrome”). Doctors aren’t stupid; they see the problem. They just had to name the problem with a certain level of science to include it in their discourse. Which, if the term is integral in the medical sphere, I can get behind it even with all my complaints about medicalization.
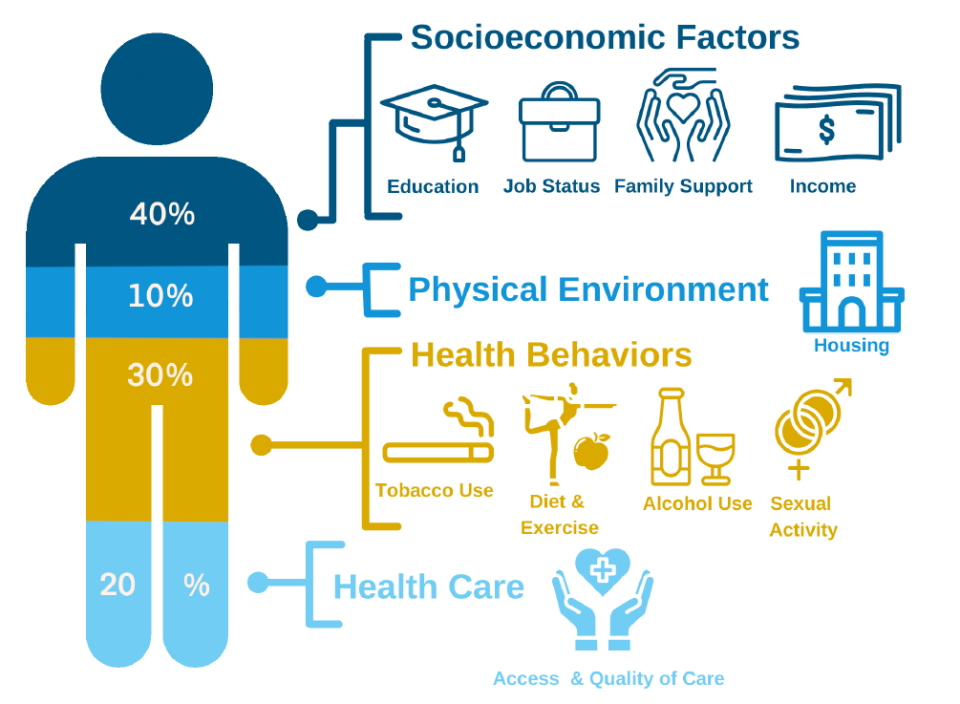
But Shit Life Syndrome, or talk about socioeconomic factors, still isn’t common in psychiatric research. Of course, the concept that “poverty often causes/correlates with poorer health outcomes” is not new. Every Medicine, Health, and Society major at Vanderbilt can quote that only 20% of a person’s overall health is determined by their access and quality of healthcare; the remaining is comprised of socioeconomic factors (40%), health behaviors (30%), and physical environment (10%). (I’ve always had an inkling that the percentage of social determinants for mental health will be even higher, but I haven’t verified that.) However, while we ask about socioeconomic circumstances during psychiatric interviews in research, the classification/diagnosis is ultimately still symptom-based.
It’s also getting worse. As many know, there have been two weeks of massive layoffs of federal workers, many of whom have careers in precisely what I just discussed (social epidemiologists, social scientists, project managers, etc.). This isn’t very encouraging, and some have even said that all these health equity and social concepts (“leftist ideals,” they said) might not exist in ten years as the world continues to go right.
Will Shit Life Syndrome ever become something we discuss as much as cognitive bias? I don’t know, but I can’t give up yet! See you next week!
Professional and Personal Notes
This week, I presented at a prestigious university’s psychiatry day, an opportunity that would have made my freshman-year self faint in excitement, but it was almost anticlimactic.
A few posters discussed non-biomedical results, which I was excited to see. One of them is a qualitative study on what instructors of psychodynamic courses have been experiencing. To no one’s surprise, they reported having to defend their views against their students’ skepticism. I told the presenter that he was brave in researching this in a biomedical environment and wished him genuine luck finding a PhD advisor to continue this work (I’m scared for him, honestly).
I also listened to the keynote lecture about what we know and don’t know about psychosis. During the Q&A, I asked this famous scholar about the Assisted-Outpatient Treatment program (a controversial bill currently in Massachusetts’s 2025 legislative session; I’ve agonized over my stance for weeks). He explained that he doesn’t have expertise in AOT programs but that 20-30% of psychosis patients “have anosognosia, which makes them unaware of their own illness.” Thus, AOT could be beneficial to them. I didn’t think of a follow-up question until later, but I’ll leave it here: if the scientists are admitting that they don’t know everything about psychosis, why is it wrong that patients can’t recognize their conditions? What conditions?
I’ll leave it at that. As always, thanks for reading!
xx Fiona